In the wake of inflation and rising healthcare costs, employers have made employee healthcare affordability a key priority. However, efforts to combat rising healthcare costs through the highest-rated utilization management (UM) tools can pose barriers to treatment.*
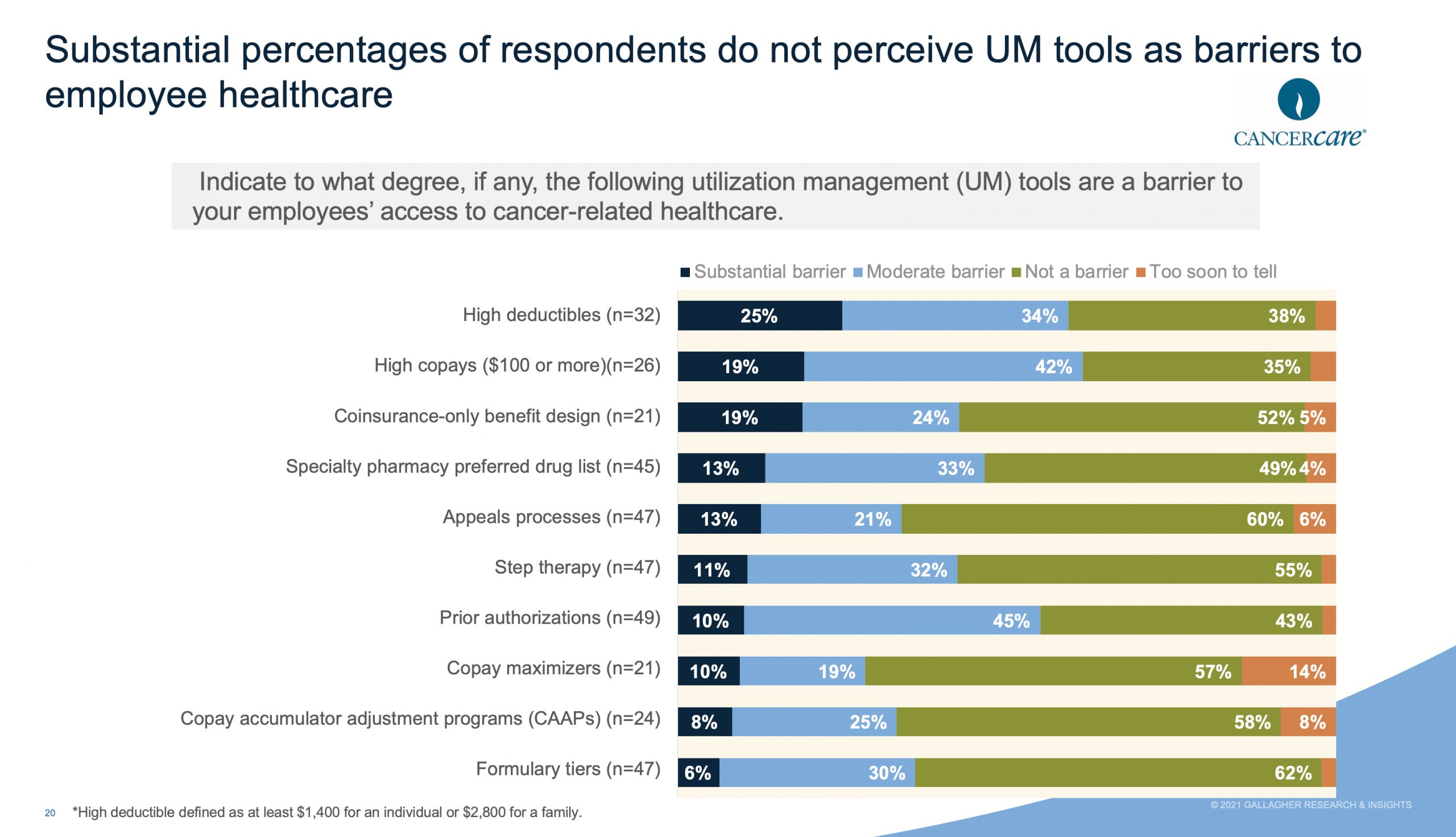
Nearly all respondents to CancerCare’s 2022 Employer Market Survey of large employers said that step therapy (96%), formulary tiers (94%), prior authorizations (94%) and specialty pharmacy preferred drug lists (92%) were very or somewhat effective in controlling costs for employees. The survey also found that a substantial number of respondents do not perceive UM tools as barriers to employees receiving the care they need, when they need it.
More than half (62%) say formulary tiers are not a barrier to care; 60% feel that the appeals process is not a barrier; 55% say step therapy is not a barrier; and 49% feel that specialty pharmacy preferred drug lists are not barriers. Many employers are unaware that, in reality, these cost-cutting measures can backfire — causing treatment delays, higher out-of-pocket costs, and non-adherence to medication, especially for individuals with serious and chronic health conditions.
“The biggest challenge employers face is designing high quality and cost-effective health plans that don’t create roadblocks to needed care,” explains Patricia Goldsmith, Chief Executive Officer, CancerCare. “No employer wants to place a burden on employees that can lead to worse outcomes, debilitating suffering, higher medical expenses, increased financial pressures, lower productivity at work, and increased absences.”
UM tactics like step therapy, formulary tiers, prior authorization and specialty pharmacy preferred drug lists may seem like attractive elements of a health plan. But as the CancerCare survey shows, many employers are unaware that these techniques can negatively impact outcomes for sick employees by causing delays to care, higher out-of-pocket costs, limited choices, and can lead to higher medical benefit costs.
“Keeping a lid on soaring healthcare costs should not be done by reducing access to needed care,” said Goldsmith. “With a better understanding of the unintended consequences of utilization management, employers can design benefit plans that allow their employees access to prompt and effective treatments while controlling overall healthcare costs.”
CancerCare recently published “The Employers’ Prescription for Employee Protection Toolkit: Best Practices for Prescription Drug Benefit Design”, to help benefits managers, human resources professionals, and executives understand and avoid the costly unintended consequences of utilization management (UM).
*CancerCare,